| Myotonic
dystrophy Classification and external resources |
|
| ICD-10 | G71.1 |
|---|---|
| OMIM | 160900 602668 |
| DiseasesDB | 8739 |
| MeSH | D009223 |
Myotonic dystrophy (DM) is a chronic, slowly progressing, highly variable inherited multisystemic disease that can manifest at any age from birth to old age. It is characterized by wasting of the muscles (muscular dystrophy), posterior subcapsular iridescent cataracts (opacity of the lens of the eyes), heart conduction defects, endocrine changes and myotonia (difficulty relaxing a muscle). Most notably, the highly variable age of onset decreases with successive generations. Thus the disease shows at an earlier age in successive generations, a phenomenon termed anticipation. There are two classifications of DM, each having different associated symptoms.
Contents[hide] |
[edit] Classification
Myotonic dystrophy is the most common form of adult onset muscular dystrophy and the second most common form of any skeletal muscle disease after Duchenne muscular dystrophy. There are currently two known types of adult onset DM, both identifiable by DNA analysis:
- Myotonic dystrophy type 1 (DM1), also known as Steinert's disease. DM1 has a congenital form that can severely affect babies and a childhood onset form.
- Myotonic dystrophy type 2 (DM2), commonly referred to as PROMM or proximal myotonic myopathy.
Further forms of myotonic dystrophy (DM3, DM4, DMX) are currently suspected by researchers to exist.[citation needed] One recent case was proposed as a candidate for the "DM3" label,[1] but was later characterized as a form of Paget's disease.[2][3]
[edit] Differences between DM1 and DM2
- While both diseases are considered slow degenerative conditions, DM2 is considered to be generally milder than DM1.
- The severe congenital form that affects babies in DM1 has not been found in DM2 and the early onset of symptoms is rarely noted to appear in younger patients in the medical literature.
- The repeat expansion for DM2 is considerably larger than for DM1, ranging from 75 to over 11,000.
- Unlike DM1, the size of the repeated DNA expansion does not appear to make a difference in the age of onset or disease severity in DM2.
- Anticipation is a common feature of DM1. It appears to be less significant in type 2 and most current reviews only report mild anticipation as a feature of DM2.
[edit] Symptoms
Presentation of symptoms varies considerably by form (DM1/DM2), severity and even unusual DM2 phenotypes. DM1 patients often present with myotonia, disabling distal weakness and severe cognitive problems. DM2 patients commonly present with muscle pain, stiffness, fatigue, or the development of proximal lower extremity weakness (Day & al, 2003). The characteristic pattern of weakness is different for DM1 and DM2: In DM1, it is noted in face and jaw muscles, the drooping of the eyelids (ptosis), weakness of the neck muscles, hands and lower legs. In DM2, the weakness is more evident in proximal muscles, those closer to the trunk of the body: neck, shoulders, hip flexors and upper legs.
Noted DM1 symptoms which are considered less severe or common for DM2 are problems with smooth muscle (including G.I. symptoms), hypersomnia (daytime sleepiness), muscle wasting, dysphagia and respiratory insufficiency. DM1 patients may experience a more diverse range of cognitive problems than DM2. Depending on what form they have and the degree of severity, DM1 cognitive problems may range from developmental delays, learning problems, language, speech, behaviour, apathy or hypersomnia. Cognitive manifestations for DM2 include problems with executive function (i.e. organization, concentration, word-finding etc) and hypersomnia. Conduction abnormalities are more common in DM1 than DM2, but all patients are advised to have an annual ECG. Insulin resistance is a significant risk factor in both forms of the disease for diabetes, cholesterol, heart, stroke, lipids, fatty liver, etc.
Testing for insulin resistance must be at least 3 hours and include serial monitoring of the lipid profile and intermittent assessment of oral glucose tolerance testing as per the report from the 140th ENMC International Workshop: Myotonic Dystrophy DM2/PROMM and other myotonic dystrophies with guidelines on management (2006) Diabetes type 2 is suspected of being more common in DM2 than in DM1. Generally far fewer DM2 patients require assistive devices (canes, walkers, wheelchairs, scooters) than in DM1, though they experience increasing difficulties climbing stairs as the disease progresses, and falling or stumbling may sometimes be reported.
[edit] Genetics
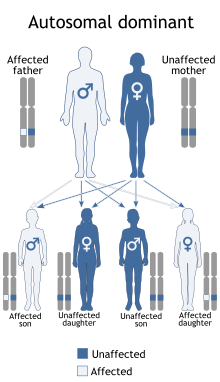
DM is a genetic condition which is inherited in an autosomal dominant pattern, meaning that inheriting a mutant gene from one parent will result in the condition. There is a 50% chance of inheriting DM from an affected parent.
DM is one of several known trinucleotide repeat disorders. Certain areas of DNA have repeated sequences of two or three nucleotides.
[edit] DM1
In DM1, the affected gene is called DMPK (myotonic dystrophy protein kinase) which codes for a myosin kinase expressed in skeletal muscle. The gene is located on the long arm of chromosome 19.
In DM1, there is a triplet repeat of Cytosine - Thymine - Guanine (CTG) in the DMPK gene. The number of repeats varies greatly from person to person, but the average number in a healthy person is between 5 and 37. Sometimes when repetitive sequences of DNA are replicated during cell division the cellular machinery slips and an extra copy of the triplet repeat is added to the sequence. Once there are more than 37 triplet repeats in the DMPK gene the sequence becomes unstable and slippage becomes a lot more likely to happen. People affected with DM1 have over 50 and can have as many as 2000 repeats.
The result of this is that the repeat size of an individual with DM1 will become larger usually during gametogenesis or early embrionic development. This explains the phenomenon of anticipation, as each child of an affected adult will have a larger expansion than their parent due to slippage during gametogenesis. Individuals with larger expansions have an earlier onset of the disorder and a more severe phenotype.
[edit] DM2
DM2 is similarly caused by a defect of the ZNF9 gene on chromosome 3q21.
The repeat expansion for DM2 is much larger than for DM1, ranging from 75 to over 11000 repeats. Unlike DM1, the size of the repeated DNA expansion does not appear to make a difference in the age of onset or disease severity in DM2. Anticipation appears to be less significant in DM2 and most current reviews only report mild anticipation as a feature of DM2.
[edit] Diagnosis
The diagnosis of DM1 and DM2 can be difficult and may be delayed due to the large number of neuromuscular disorders, most of which are very rare. Neuromuscular disorders can cover more than 40 different diseases and additional forms of these bring the number of distinct disorders close to 100.
As a result, patients with multiple symptoms that may be explained by a complex disorder such as DM1 or DM2 will generally be referred by their family doctor to a neuromuscular specialist for diagnosis. Depending on the presentation of symptoms, patients may be referred to a number of medical specialists including cardiologists, ophthalmologists, endocrinologists, rheumatologists. In addition, the clinical presentation varies considerably depending on the degree of severity or the presence of unusual phenotypes, so making diagnosis even more difficult.
Some neuromuscular specialists focus primarily on many of the childhood onset neuromuscular diseases, while others may have research and clinical interests focused on specific diseases such as ALS and may be unaware of the potential relationship of specific symptoms to DM.
It is common that the clinical presentation for both DM1 and DM2 patients does not conform to the perceptions of these diseases held by many neurologists. Clinicians who are less familiar with the myotonic dystrophies in their day to day practice may expect patients with both forms to present with the more severe classic symptoms of DM1. As a result, patients may remain undiagnosed or be misdiagnosed.
Even though there is presently no cure for DM and management is currently symptom based, a precise diagnosis is still necessary because of multiple other problems that may develop over time. Even mildly affected DM1 & DM2 patients should be routinely monitored for potentially fatal complications (i.e. cardiac conduction issues, insulin resistance, cataracts). An accurate diagnosis is important to assist with appropriate medical monitoring and medical management of symptoms. In addition, genetic counseling should be made available to all patients because of the high risk of transmission. Potentially serious anesthetic risks are important to note, so the presence of this disorder should be brought to the attention of all medical providers.
[edit] Management
There is currently no cure for or treatment specific to myotonic dystrophy. Heart problems, cataracts, and other abnormalities associated with the condition can be treated but not cured. However there are medical interventions and medications that may relieve some of the symptoms such as myotonia, pain and excessive sleepiness. Some treatments have been subject to systematic review for safety and efficacy through the Cochrane Reviews for symptoms such as hypersomnia (excessive daytime sleepiness), myotonia, strength training and aerobic exercise training and foot drop.
Recent research has provided more information on the underlying molecular pathomechanisms involved in myotonic dystrophy and has fueled interest and research into new approaches for more specific and effective treatment. Research in areas such as high throughput screening and antisense therapy hold hope for more effective targeted treatments for the future. Altered splicing of the muscle-specific chloride channel 1 (ClC-1) has been shown to cause the myotonic phenotype of DM1 and is reversible in mouse models using Morpholino antisense to modify splicing of ClC-1 mRNA[4].
Progress in this area is being fueled by the sharing of research by scientists and clinicians at biannual meetings by the International Myotonic Dystrophy Consortium (IDMC). The 6th meeting (IDMC-6) took place in Milan Italy in September 2007.
[edit] Screening
Screening for the DMPK gene for DM1 is targeted at chromosome 19 while the ZNF9 gene for DM2 is found on chromosome 3. Genetic tests are available for both confirmed forms. Molecular testing is considered the gold standard of diagnosis. Further forms of myotonic dystrophy (DM3, DM4, DMX) are suspected by researchers with possible defects on chromosome 16 and chromosome 21.
[edit] Recommended Reading
- Sir Peter S. Harper,. Myotonic Dystrophy: The Facts : A Book for Patients and Families (Oxford Medical Publications). Oxford [Oxfordshire]: Oxford University Press. ISBN 0-19-852586-9.
- Peter S. Harper... [et al.] (2004). Myotonic dystrophy: present management, future therapy. Oxford [Oxfordshire]: Oxford University Press. ISBN 0-19-852782-9.
- Robert D. Wells (Editor), Tetsuo Ashizawa (Editor). Genetic Instabilities and Neurological Diseases, Second Edition, 2006. Boston: Academic Press. ISBN 0-12-369462-0. This book has chapters on multiple disorders including both Steinerts (DM1) and PROMM (DM2). The revised 2006 edition is the first print resource to have a full chapter on DM2: Myotonic Dystrophy Type 2: Clinical and Genetic Aspects by Krahe, Bachinski, and Udd This book is intended to be a reference for medical professionals such as neurologists, neuroscientists, biochemists, geneticists, molecular biologists & human geneticists.
[edit] Research and Reviews
The research on DM1/DM2/DM3 has rapidly evolved over the last decade. Always note dates of research or the update period for websites to provide context for how current and accurate the information may be. Although the newest research is rarely available without journal subscription, there are many free online reports and reviews which discuss the clinical spectrum of symptoms, therapies, etc for both DM1 and DM2. These papers are a collaborative effort by those on the front lines to document the current state of research and should be used as a resource by doctors for guidance on diagnosis and management.
- Ranum LP, Day JW (2004). "Myotonic dystrophy: RNA pathogenesis comes into focus". Am. J. Hum. Genet. 74 (5): 793804. doi:. PMID 15065017.
- van Engelen BG, Eymard B, Wilcox D (2005). "123rd ENMC International Workshop: management and therapy in myotonic dystrophy, 6-8 February 2004, Naarden, The Netherlands". Neuromuscul. Disord. 15 (5): 38994. doi:. PMID 15833434.
- Udd B, Meola G, Krahe R, et al (2006). "140th ENMC International Workshop: Myotonic Dystrophy DM2/PROMM and other myotonic dystrophies with guidelines on management". Neuromuscul. Disord. 16 (6): 40313. doi:. PMID 16684600.
- The 6th International Myotonic Dystrophy Consortium (IDMC-6)2007
[edit] References
- ^ Le Ber I, Martinez M, Campion D, et al (2004). "A non-DM1, non-DM2 multisystem myotonic disorder with frontotemporal dementia: phenotype and suggestive mapping of the DM3 locus to chromosome 15q21-24". Brain 127 (Pt 9): 197992. doi:. PMID 15215218.
- ^ "Myotonic Dystrophy Type 2". Retrieved on 2008-02-24.
- ^ Udd B, Meola G, Krahe R, et al (2006). "140th ENMC International Workshop: Myotonic Dystrophy DM2/PROMM and other myotonic dystrophies with guidelines on management". Neuromuscul. Disord. 16 (6): 40313. doi:. PMID 16684600.
- ^ Wheeler TM, Lueck JD, Swanson MS, Dirksen RT, Thornton CA (2007). "Correction of ClC-1 splicing eliminates chloride channelopathy and myotonia in mouse models of myotonic dystrophy". J. Clin. Invest. 117 (12): 39527. doi:. PMID 18008009.
[edit] External links
- Overview of condition at NLM Genetics Home Reference
- Searchable database at Dutch Neuromuscular Research
- 140th ENMC International Workshop 2006 Myotonic Dystrophy DM2/PROMM and other Myotonic dystrophies]
- Information from the International Myotonic Dystrophy Organization
- MDSG Information
- Information from the Neuromuscular Disease Center
|
||||||||||||||||||||